Signs of perimenopause – Embark on a journey through the complexities of perimenopause, a pivotal stage marked by an array of physical, emotional, and hormonal shifts. This comprehensive guide unravels the intricacies of this transition, empowering individuals to navigate its challenges with knowledge and resilience.
As the body prepares for menopause, perimenopause brings forth a multitude of changes that can impact various aspects of life. From subtle shifts in mood to more pronounced physical symptoms, this guide provides an in-depth exploration of the telltale signs associated with this phase.
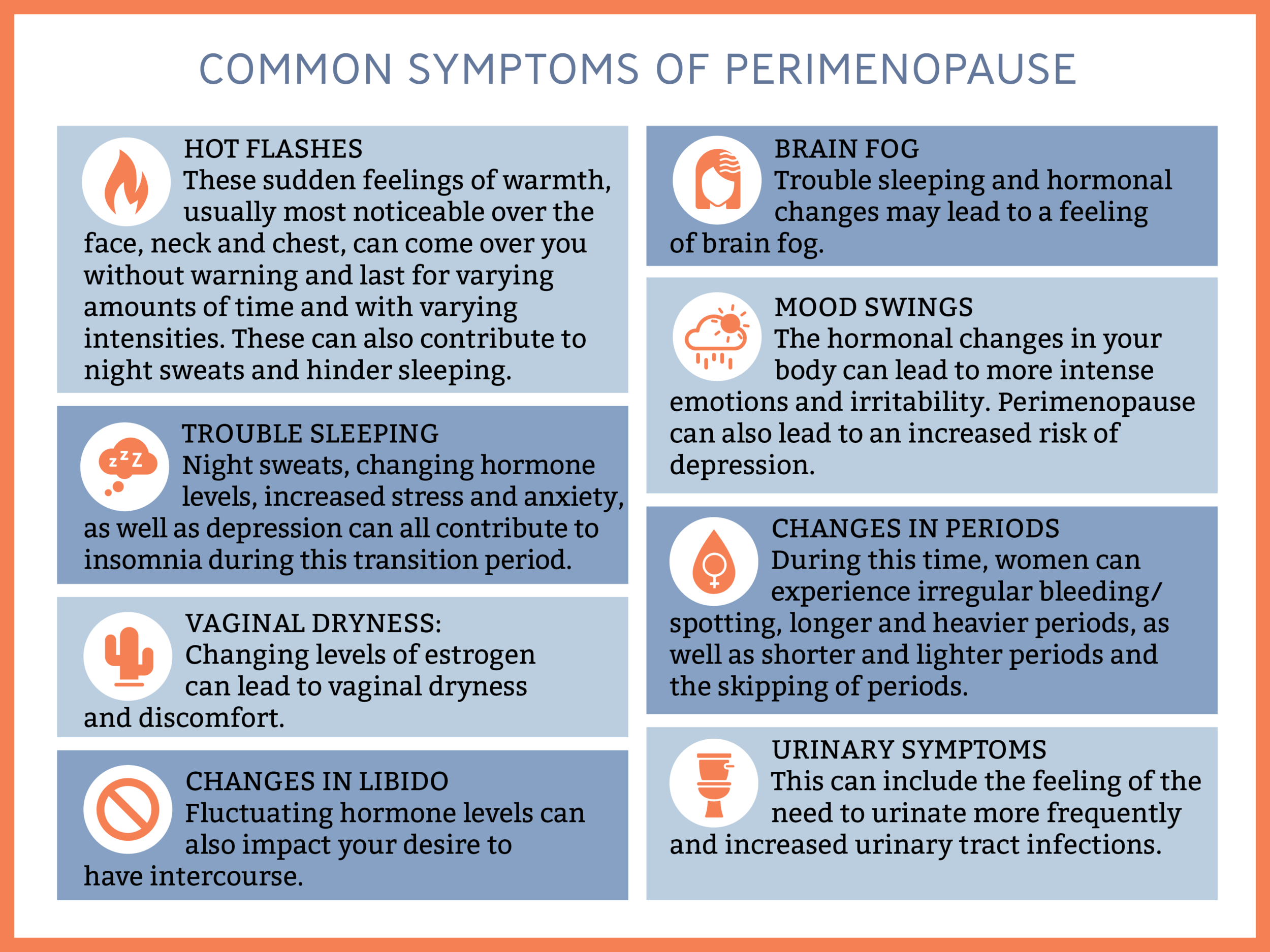
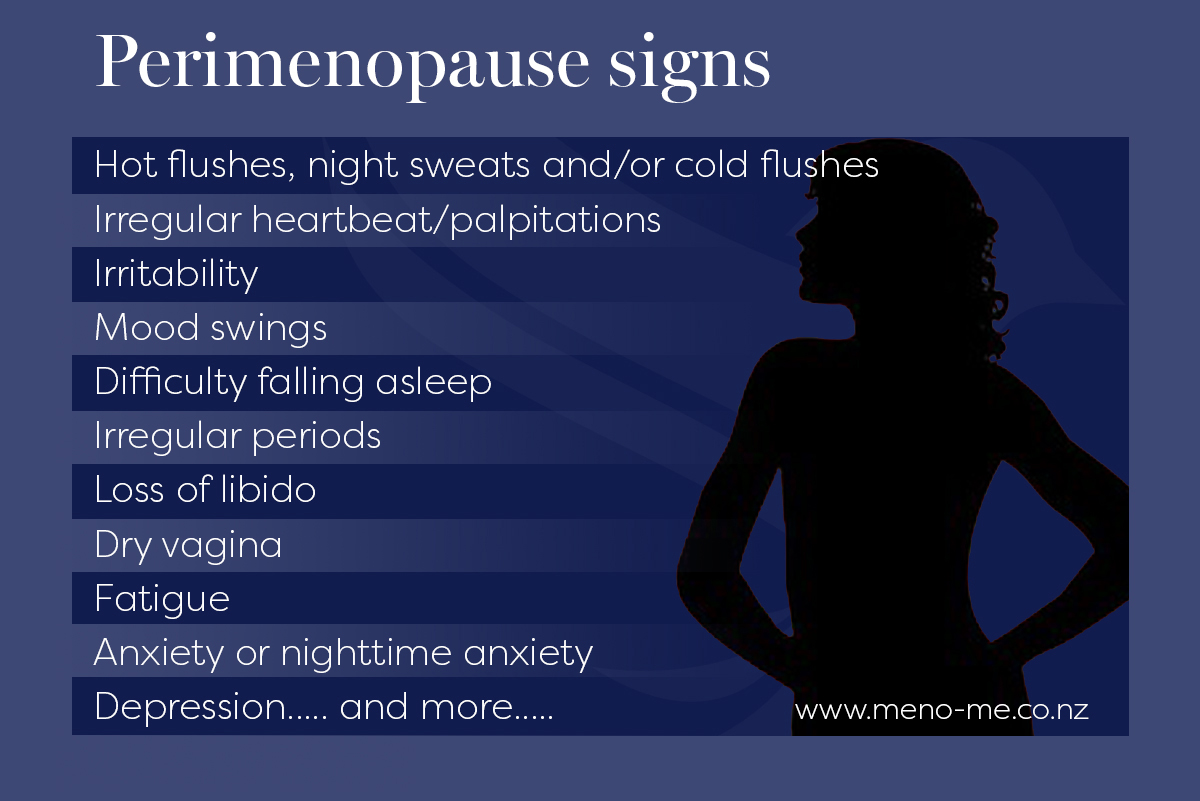
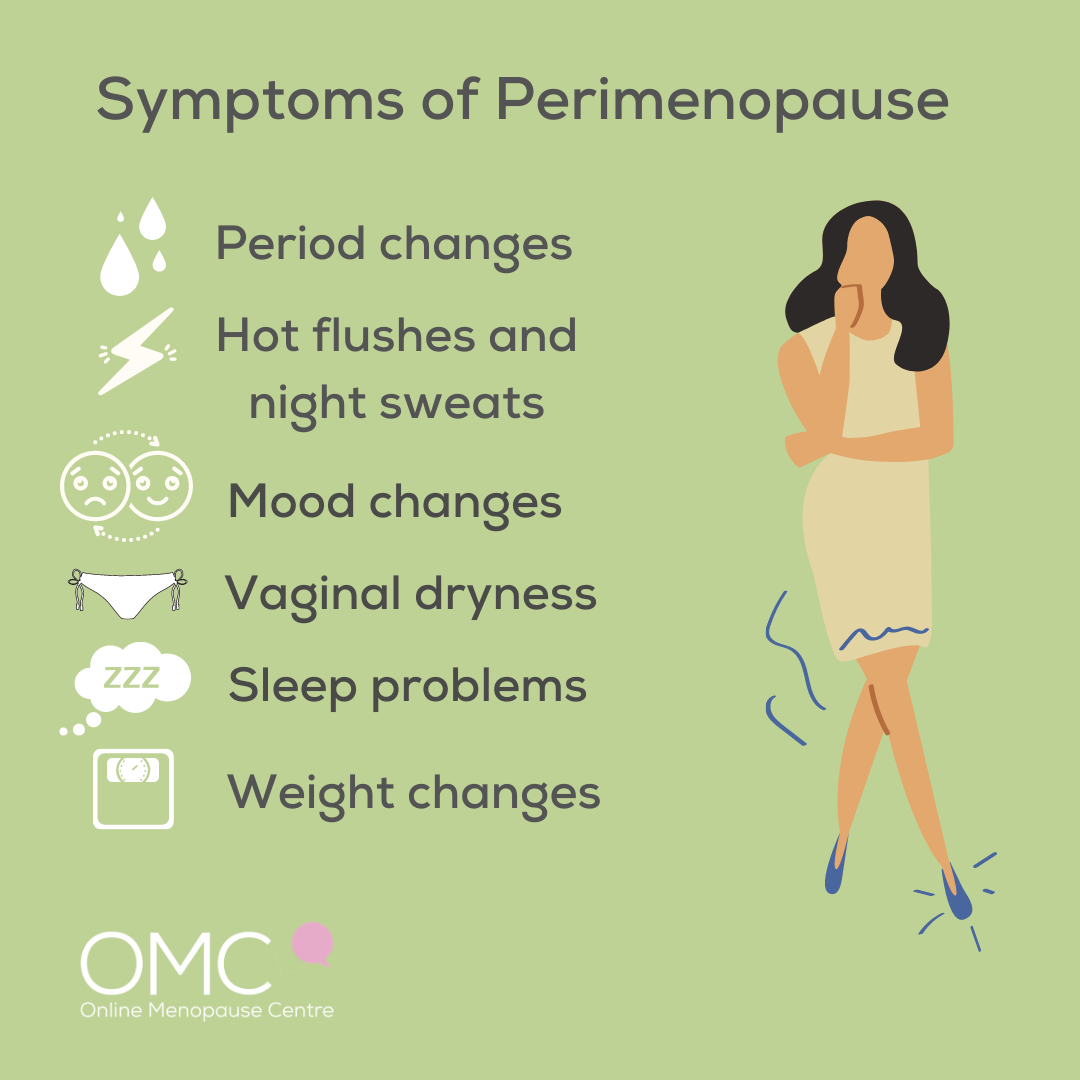
Physical Symptoms
Perimenopause, the transition to menopause, is marked by a decline in estrogen levels. This hormonal shift triggers various physical changes, including:
Hot Flashes and Night Sweats
- Sudden feelings of intense heat and sweating, often accompanied by flushing and redness of the face and neck.
- Can occur at any time of day or night, but are more common at night.
Irregular Periods
- Periods may become more frequent, less frequent, or skip altogether.
- Flow may be heavier or lighter than usual.
Sleep Disturbances
- Difficulty falling or staying asleep.
- Waking up frequently at night.
- Early morning awakenings.
Mood Changes
- Irritability, mood swings, and anxiety.
- Difficulty concentrating and memory lapses.
Other Symptoms
- Vaginal dryness.
- Breast tenderness.
- Weight gain.
- Headaches.
- Fatigue.
The frequency and severity of these symptoms vary from person to person.
| Symptom | Frequency |
|---|---|
| Hot flashes and night sweats | 50-80% |
| Irregular periods | 40-50% |
| Sleep disturbances | 30-50% |
| Mood changes | 20-30% |
| Other symptoms | 10-20% |
Emotional Symptoms
Perimenopause can bring about a range of emotional changes due to the hormonal fluctuations occurring during this transition. These changes can impact mood, sleep, and relationships.
Mood swings are a common symptom of perimenopause. Estrogen and progesterone, hormones that regulate mood, fluctuate significantly during this time, leading to feelings of irritability, anxiety, or depression. Sleep disturbances are also prevalent, as hormonal changes can disrupt the body’s natural sleep-wake cycle.
This can result in insomnia, difficulty falling asleep, or waking up frequently during the night.
Impact on Relationships, Signs of perimenopause
Emotional changes associated with perimenopause can also affect relationships. Mood swings and irritability can put a strain on personal interactions, while sleep deprivation can contribute to fatigue and decreased energy levels, making it challenging to engage in meaningful connections. It is important for individuals experiencing these symptoms to communicate openly with their partners and loved ones to seek understanding and support.
Hormonal Changes
Perimenopause is a transitional phase in a woman’s life marked by a decline in reproductive hormones, primarily estrogen and progesterone.
As the ovaries gradually reduce hormone production, the levels of estrogen and progesterone fluctuate erratically, leading to a wide range of physical, emotional, and hormonal changes.
Estrogen and Progesterone Fluctuations
During perimenopause, estrogen levels fluctuate significantly, with periods of high and low estrogen.
- High Estrogen:Estrogen levels may initially increase during perimenopause due to the body’s attempts to compensate for the decline in hormone production.
- Low Estrogen:As perimenopause progresses, estrogen levels gradually decline, leading to symptoms such as hot flashes, vaginal dryness, and irregular periods.
Progesterone levels also decline during perimenopause, but the fluctuations are typically less pronounced than those of estrogen.
The following table illustrates the general pattern of estrogen and progesterone fluctuations during perimenopause:
| Phase | Estrogen | Progesterone |
|---|---|---|
| Early Perimenopause | Variable | Variable |
| Mid Perimenopause | Fluctuating, declining | Declining |
| Late Perimenopause | Low | Low |
Management Strategies
Managing perimenopause symptoms requires a multifaceted approach that addresses both physical and emotional changes. Lifestyle modifications, dietary adjustments, and potential therapies can effectively alleviate discomfort and improve overall well-being.
Lifestyle Modifications:
- Regular exercise: Engage in moderate-intensity exercise for at least 30 minutes most days of the week. Exercise helps reduce stress, improve mood, and strengthen bones.
- Healthy diet: Focus on consuming a balanced diet rich in fruits, vegetables, whole grains, and lean protein. Limit processed foods, sugary drinks, and excessive caffeine.
- Adequate sleep: Aim for 7-9 hours of quality sleep each night. Establish a regular sleep schedule and create a relaxing bedtime routine.
- Stress management: Engage in stress-reducing activities such as yoga, meditation, or deep breathing exercises. Managing stress can help regulate hormonal fluctuations.
- Social support: Connect with family, friends, or support groups to share experiences and provide emotional support.
Dietary Recommendations:
- Phytoestrogens: Include foods rich in phytoestrogens, such as soybeans, flaxseeds, and tofu, which may help balance estrogen levels.
- Calcium and vitamin D: Ensure adequate intake of calcium and vitamin D to maintain bone health and reduce the risk of osteoporosis.
- Omega-3 fatty acids: Consume foods high in omega-3 fatty acids, such as salmon, tuna, or walnuts, to reduce inflammation and improve mood.
Potential Therapies:
- Hormone therapy: Hormone therapy, including estrogen and progestin, can help alleviate hot flashes, night sweats, and vaginal dryness.
- Antidepressants: Certain antidepressants, such as selective serotonin reuptake inhibitors (SSRIs), can improve mood and reduce anxiety associated with perimenopause.
- Herbal supplements: Some herbal supplements, such as black cohosh and red clover, may help manage hot flashes and other symptoms. However, it is crucial to consult a healthcare professional before using herbal supplements.
Medical Considerations: Signs Of Perimenopause
Medical evaluation during perimenopause is crucial for several reasons. It helps confirm the diagnosis, rule out underlying medical conditions, and assess the need for treatment options. A comprehensive evaluation typically involves a physical exam, blood tests, and a discussion of symptoms.
One of the primary considerations during perimenopause is the potential risks and benefits of hormone replacement therapy (HRT). HRT involves taking synthetic hormones to replace the declining levels of estrogen and progesterone during menopause. While HRT can effectively alleviate symptoms like hot flashes, night sweats, and vaginal dryness, it also carries potential risks such as increased risk of blood clots, stroke, and certain types of cancer.
The decision of whether or not to pursue HRT should be made in consultation with a healthcare professional after weighing the individual’s specific needs and risks.
Hormone Replacement Therapy
- Estrogen-only HRT: May be prescribed to women who have had a hysterectomy or are at high risk of breast cancer.
- Combined HRT (estrogen and progestin): May be prescribed to women who still have their uterus to protect against endometrial cancer.
- Transdermal HRT (patches, gels, or creams): May be an alternative to oral HRT for women who experience gastrointestinal side effects.
Detailed FAQs
What is the average age for perimenopause?
Perimenopause typically begins between the ages of 45 and 55.
How long does perimenopause last?
Perimenopause can last anywhere from a few months to several years.
What are the most common physical symptoms of perimenopause?
Common physical symptoms include hot flashes, night sweats, vaginal dryness, and irregular periods.
What are the most common emotional symptoms of perimenopause?
Common emotional symptoms include mood swings, irritability, anxiety, and difficulty sleeping.