Hysterectomy and menopause are two significant life events that can have a profound impact on a woman’s physical, emotional, and psychological well-being. Understanding the relationship between these two events is crucial for women navigating this transition. This article delves into the complexities of hysterectomy and menopause, providing comprehensive information and guidance to help women make informed decisions and manage the challenges they may face.
A hysterectomy is a surgical procedure to remove the uterus, and in some cases, the ovaries and fallopian tubes. Menopause is the natural cessation of menstruation, which typically occurs between the ages of 45 and 55. While hysterectomy and menopause are distinct events, they can be interconnected, as a hysterectomy can trigger menopause if the ovaries are removed during the procedure.
Definition of Hysterectomy and Menopause

A hysterectomy is a surgical procedure that removes the uterus, and sometimes the cervix, fallopian tubes, and ovaries. It is typically performed to treat conditions such as uterine fibroids, endometriosis, and cancer.
Menopause is the natural process by which a woman’s ovaries stop producing eggs and her menstrual periods cease. It typically occurs between the ages of 45 and 55.
A hysterectomy can induce menopause if the ovaries are removed during the procedure. This is because the ovaries produce the hormones estrogen and progesterone, which are responsible for regulating the menstrual cycle.
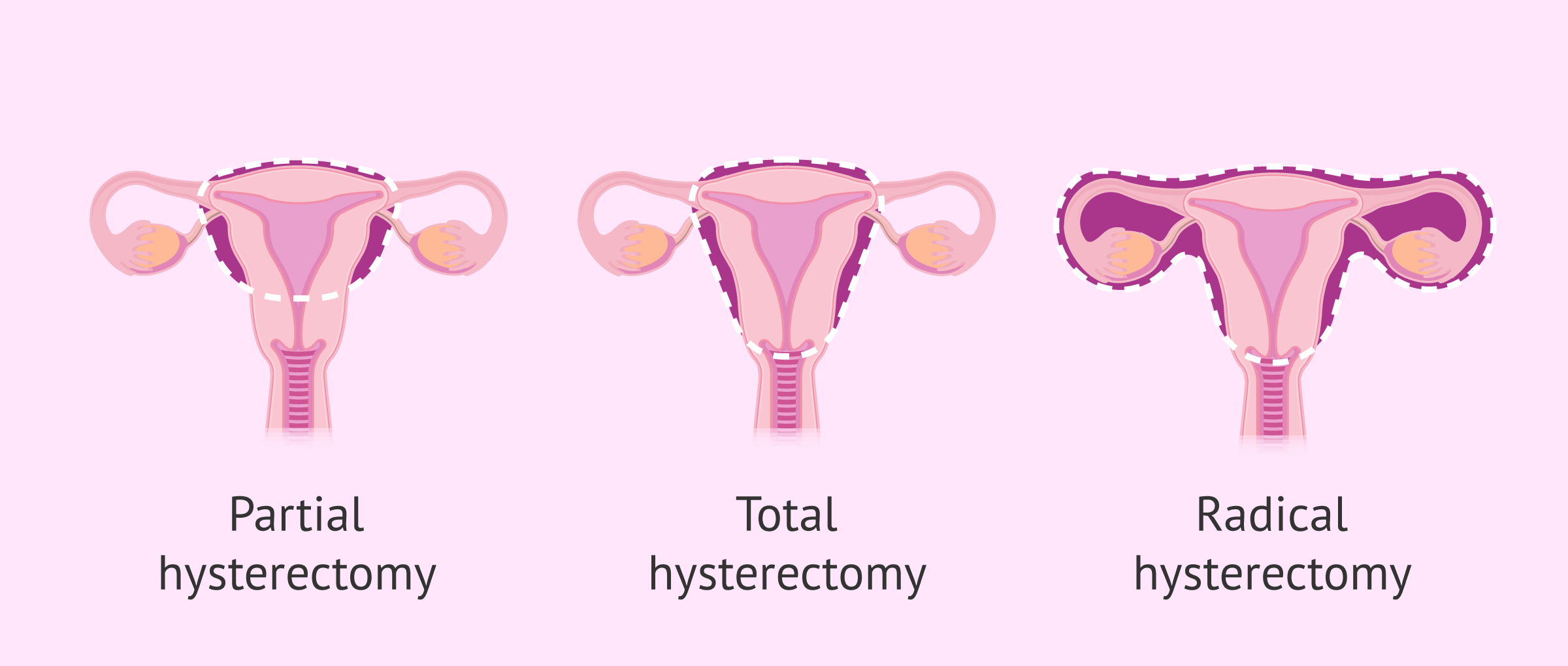
Types of Hysterectomies
- Total hysterectomy:Removes the uterus, cervix, and fallopian tubes.
- Subtotal hysterectomy (also known as supracervical hysterectomy):Removes the uterus but leaves the cervix intact.
- Radical hysterectomy:Removes the uterus, cervix, fallopian tubes, ovaries, and surrounding lymph nodes.
Impact of Hysterectomy on Menopause: Hysterectomy And Menopause
A hysterectomy, the surgical removal of the uterus, can have a significant impact on menopause, the natural process of hormonal changes that marks the end of a woman’s reproductive years. Understanding these effects is crucial for women considering or undergoing a hysterectomy.
A hysterectomy typically involves the removal of the ovaries, which are responsible for producing the hormones estrogen and progesterone. These hormones play a vital role in regulating a woman’s menstrual cycle and maintaining overall health. When the ovaries are removed, hormone production ceases abruptly, triggering menopause.
Changes in Hormone Levels
- Estrogen:Estrogen levels drop dramatically after a hysterectomy, leading to symptoms such as hot flashes, night sweats, vaginal dryness, and mood swings.
- Progesterone:Progesterone levels also decline, which can contribute to irregular bleeding, weight gain, and difficulty sleeping.
Symptoms Associated with Menopause After a Hysterectomy
- Hot flashes:Sudden feelings of intense heat that can cause sweating, flushing, and palpitations.
- Night sweats:Hot flashes that occur during sleep, causing discomfort and sleep disturbances.
- Vaginal dryness:Decreased estrogen levels can lead to thinning and dryness of the vaginal walls, resulting in discomfort during intercourse and an increased risk of infections.
- Mood swings:Hormonal fluctuations can trigger emotional instability, irritability, and mood swings.
- Weight gain:Declining estrogen levels can slow down metabolism and increase fat storage, leading to weight gain.
- Osteoporosis:Estrogen plays a crucial role in bone health. Its deficiency after a hysterectomy can increase the risk of osteoporosis, a condition that weakens bones and makes them more susceptible to fractures.
Comparison to Natural Menopause
The experience of menopause after a hysterectomy differs from natural menopause in several ways:
- Sudden onset:Natural menopause is a gradual process that occurs over several years, whereas menopause after a hysterectomy is sudden and immediate.
- Severity of symptoms:Symptoms of menopause after a hysterectomy are often more severe and persistent than those of natural menopause due to the abrupt drop in hormone levels.
- Long-term effects:Women who undergo a hysterectomy may experience long-term effects, such as an increased risk of osteoporosis and heart disease, due to the permanent loss of estrogen production.
Treatment Options for Menopausal Symptoms after Hysterectomy

After a hysterectomy, women may experience menopausal symptoms due to the loss of estrogen production. These symptoms can include hot flashes, night sweats, vaginal dryness, and mood swings. There are several treatment options available to help alleviate these symptoms.
Hormone Replacement Therapy (HRT)
HRT is a common treatment option for menopausal symptoms. It involves taking synthetic hormones to replace the estrogen and progesterone that are no longer being produced by the ovaries. HRT can be taken in various forms, including pills, patches, and injections.
Benefits of HRT:
- Relieves hot flashes and night sweats
- Reduces vaginal dryness
- Improves mood and sleep
- Protects against osteoporosis
Risks of HRT:
- Increased risk of breast cancer
- Increased risk of blood clots
- Increased risk of stroke
- Nausea and vomiting
Alternative Treatment Options, Hysterectomy and menopause
For women who cannot or do not want to take HRT, there are alternative treatment options available. These include:
- Lifestyle changes, such as exercise, diet, and stress management
- Over-the-counter medications, such as ibuprofen or acetaminophen
- Prescription medications, such as antidepressants or anti-anxiety medications
- Herbal remedies, such as black cohosh or red clover
Emotional and Psychological Effects of Hysterectomy and Menopause
Hysterectomy and menopause can have a profound impact on a woman’s emotional and psychological well-being. These life-altering events can trigger feelings of loss, grief, and a sense of change in identity.
Feelings of Loss and Grief
A hysterectomy involves the surgical removal of the uterus, which can lead to feelings of loss and grief. This is particularly true for women who have not yet had children or who had hoped to have more children. The loss of the uterus can also symbolize a loss of femininity and fertility.
Impact of Hormonal Changes
Menopause, which typically occurs naturally around age 51, involves a decline in the production of estrogen and progesterone. These hormonal changes can affect mood, sleep, and overall well-being. Women may experience mood swings, irritability, anxiety, and depression. They may also have difficulty concentrating and remembering things.
Coping Mechanisms
Coping with the emotional and psychological challenges of hysterectomy and menopause requires a multifaceted approach. It is important for women to acknowledge and validate their feelings of loss and grief. They may find it helpful to talk to a therapist or counselor to process these emotions.
Additionally, there are a number of lifestyle changes that can help improve mood and well-being, such as:
- Regular exercise
- Healthy diet
- Adequate sleep
- Stress-reducing activities
- Social support
Long-Term Health Implications of Hysterectomy and Menopause
Hysterectomy and menopause, while often medically necessary, can have long-term health implications that women should be aware of. Understanding these implications is crucial for proactive health management and maintaining well-being in the years following these events.
One significant concern is the increased risk of osteoporosis, a condition characterized by weakened and brittle bones. Estrogen, a hormone produced by the ovaries, plays a vital role in maintaining bone density. After menopause, when estrogen levels decline, women experience a decrease in bone mass, making them more susceptible to osteoporosis.
Similarly, hysterectomy, which involves the removal of the uterus and often the ovaries, can lead to an earlier onset of menopause and, consequently, an increased risk of osteoporosis.
Another potential long-term implication is an elevated risk of cardiovascular disease. Estrogen has protective effects on the heart and blood vessels. After menopause or hysterectomy, the loss of estrogen can contribute to the development of cardiovascular conditions such as heart disease and stroke.
Women who have undergone hysterectomy and menopause should be particularly vigilant about maintaining a healthy lifestyle, including regular exercise, a balanced diet, and not smoking, to mitigate this risk.
Importance of Regular Check-Ups and Screenings
Regular check-ups and screenings are essential for women who have undergone hysterectomy and menopause. These appointments allow healthcare providers to monitor overall health, assess bone density, and screen for potential health issues. Bone density screenings, such as dual-energy X-ray absorptiometry (DEXA) scans, can help detect osteoporosis early on, enabling timely intervention to prevent fractures and maintain bone health.
Additionally, regular mammograms and Pap tests are recommended to screen for breast and cervical cancer, respectively.
Maintaining a Healthy Lifestyle After Hysterectomy and Menopause
Adopting a healthy lifestyle after hysterectomy and menopause is crucial for long-term well-being. Regular exercise, particularly weight-bearing exercises such as walking, running, or dancing, helps maintain bone density and reduces the risk of osteoporosis. A balanced diet rich in calcium and vitamin D is essential for bone health.
Calcium can be obtained from dairy products, leafy green vegetables, and fortified foods, while vitamin D is found in fatty fish, eggs, and fortified milk. Quitting smoking and limiting alcohol consumption are also beneficial for overall health and well-being.
Decision-Making and Informed Consent
Undergoing a hysterectomy is a significant decision that requires careful consideration and informed consent. Informed consent involves providing patients with comprehensive information about the procedure, its potential benefits and risks, and alternative treatment options. It empowers patients to make informed decisions about their healthcare and ensures that they understand the implications of the procedure.
Factors to Consider
When making a decision about hysterectomy, several factors should be taken into account:
- Medical condition:The underlying medical condition, such as uterine fibroids, endometriosis, or cancer, and its severity.
- Symptoms:The severity and impact of the symptoms associated with the medical condition.
- Age and reproductive goals:The patient’s age and whether they desire future pregnancies.
- Alternative treatments:The availability and effectiveness of alternative treatments for the medical condition.
- Personal values and preferences:The patient’s personal values, beliefs, and preferences regarding the procedure.
Role of Healthcare Professionals
Healthcare professionals play a crucial role in providing patients with the necessary information and support to make informed decisions. They should:
- Discuss the medical condition, its symptoms, and the rationale for hysterectomy.
- Explain the procedure, its potential benefits, risks, and complications.
- Provide information about alternative treatment options and their effectiveness.
- Address the patient’s concerns and answer their questions.
- Respect the patient’s values, preferences, and decisions.
Legal and Ethical Considerations
Hysterectomy is a surgical procedure that requires legal and ethical considerations:
- Consent:Informed consent is a legal requirement before performing a hysterectomy.
- Patient autonomy:Patients have the right to make decisions about their own bodies and healthcare.
- Medical necessity:Hysterectomy should only be performed when medically necessary and when alternative treatments are not effective.
- Ethical guidelines:Healthcare professionals must adhere to ethical guidelines and standards of care when performing hysterectomies.
FAQ Resource
What is the difference between natural menopause and surgical menopause?
Natural menopause occurs gradually over several years, while surgical menopause is the immediate cessation of menstruation after a hysterectomy that removes the ovaries.
What are the common symptoms of menopause after a hysterectomy?
Hot flashes, night sweats, vaginal dryness, mood swings, and sleep disturbances are common symptoms of menopause after a hysterectomy.
What are the treatment options for menopausal symptoms after a hysterectomy?
Hormone replacement therapy (HRT) is the most common treatment for menopausal symptoms after a hysterectomy. Other options include lifestyle modifications, alternative therapies, and prescription medications.